Few dental topics generate as much confusion as wisdom teeth. While some people view their removal as an inevitable rite of passage, others question whether extraction is always necessary. At Vident Dental Clinic, we believe in evidence-based approaches to third molar management, recognizing that each patient's situation requires individualized assessment rather than a one-size-fits-all solution.
This comprehensive guide explores current research on wisdom teeth, helping you understand when removal is truly beneficial and when watchful waiting may be appropriate.
Understanding Wisdom Teeth: The Evolutionary Perspective
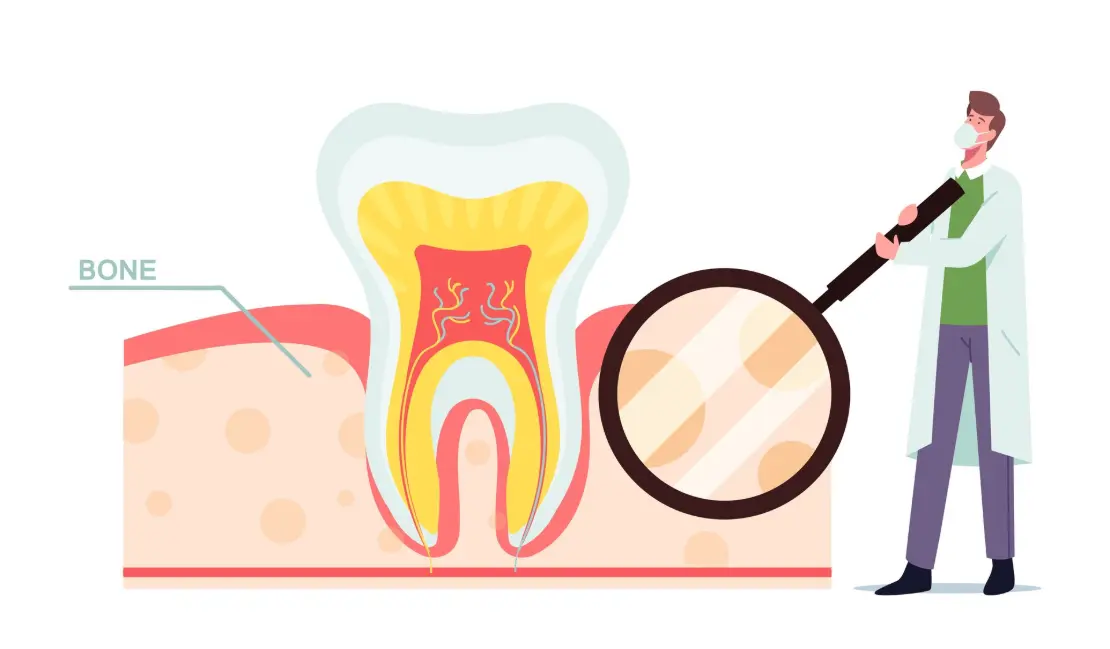
Third molars, commonly known as wisdom teeth, typically emerge between ages 17-25—hence their name, as they appear during the "age of wisdom." These final additions to your dental collection have an interesting evolutionary history.
Why We Have Them
Anthropologists believe wisdom teeth served important functions for our ancestors:
- Replacement teeth: They provided backup chewing surfaces when other teeth were lost
- Stronger jaws: Early humans had larger, more powerful jaws that accommodated these extra molars
- Coarse diet: Fibrous, unprocessed foods required additional grinding surfaces
Modern humans have experienced significant changes in both jaw structure and diet, creating the current mismatch between our anatomy and these evolutionary holdovers.
The Contemporary Challenge
Several factors contribute to wisdom tooth complications in modern humans:
- Smaller jaws: Evolution has reduced jaw size, creating space limitations
- Refined diet: Softer foods have decreased jaw development stimulation
- Dental care: Better oral hygiene and dentistry have reduced tooth loss, eliminating the need for "backup" molars
- Facial structure changes: Modern human facial development creates different eruption patterns
These factors explain why approximately 70% of people experience some form of wisdom tooth impaction or eruption difficulty. However, this statistic also indicates that 30% may have normally erupting third molars that function without problems.
The Evidence-Based Approach to Wisdom Teeth
Current dental research supports a more nuanced approach to third molar management than the blanket "extract them all" philosophy that prevailed in previous decades.
When Removal Is Clearly Indicated
Research supports extraction in several specific circumstances:
- Infection or pericoronitis: Recurring inflammation of the tissue surrounding partially erupted wisdom teeth
- Progressive periodontal disease: Bone loss that cannot be arrested with conservative measures
- Caries without restoration potential: Decay that cannot be effectively treated
- Cysts or tumors: Pathological changes in the follicular tissue surrounding unerupted teeth
- Damage to adjacent teeth: Resorption or decay of neighboring second molars
- Chronic pain: Persistent discomfort attributable to the third molars
- Severe impaction with future risk: Horizontal or mesioangular impactions likely to cause problems
A systematic review in the Cochrane Database found that in these situations, the benefits of removal clearly outweigh the risks of retention.
When Monitoring May Be Appropriate
Evidence suggests that asymptomatic wisdom teeth may be candidates for retention and monitoring when:
- Fully erupted: Teeth that have completely emerged into functional position
- Proper alignment: Third molars in normal occlusion with opposing teeth
- Adequate cleaning access: Positioning that allows effective hygiene
- Healthy surrounding tissues: No evidence of periodontal disease or inflammation
- No pathology: Absence of cysts or other abnormalities on radiographs
- Completed root development: Fully formed roots in favorable positions
A longitudinal study published in the Journal of Oral and Maxillofacial Surgery followed asymptomatic third molars for over 25 years, finding that many remained disease-free when these conditions were met and proper monitoring continued.
The Middle Ground: Situations Requiring Careful Assessment
Many cases fall into a gray area requiring individualized risk-benefit analysis:
- Partially erupted teeth: May or may not cause future problems depending on orientation
- Impacted but asymptomatic teeth: Require evaluation of long-term risk
- Orthodontic considerations: May factor into decisions about crowding or stability
- Medical history factors: Systemic conditions that might complicate either retention or removal
- Age considerations: Different risk-benefit ratios at various life stages
In these situations, decisions should incorporate both clinical evidence and patient preferences after thorough discussion of potential outcomes.
Risk Assessment: Predicting Future Problems
Several factors help predict whether asymptomatic wisdom teeth might cause issues later.
Positional Analysis
The orientation of wisdom teeth significantly affects their prognosis:
- Vertical impaction: Generally has better outcomes if partial eruption allows cleaning
- Mesioangular impaction: Tilted toward the second molar, creating higher risk for food traps and decay
- Horizontal impaction: Positioned sideways, associated with higher complication rates
- Distoangular impaction: Angled backward, often more challenging to extract but may cause fewer problems if asymptomatic
Radiographic analysis of these positions helps determine risk levels for future complications.
Soft Tissue Configuration
The relationship between the wisdom tooth and surrounding soft tissues affects infection risk:
- Operculum coverage: Partial soft tissue coverage creates pockets where bacteria accumulate
- Pseudopocket depth: Deeper tissue pockets around partially erupted teeth increase infection risk
- Accessibility: Location relative to the cheek and tongue affects cleaning ability
- Tissue thickness: Thicker tissue may be more prone to traumatic irritation
These factors help predict the likelihood of developing pericoronitis, a common indication for extraction.
Age-Related Considerations
The patient's age influences both risk assessment and treatment recommendations:
- Adolescents (15-18): Root development incomplete, extraction technically easier but necessity less certain
- Young adults (19-25): Optimal surgical timing if indicated, with faster healing and fewer complications
- Adults (26-35): Increased surgical complexity as bone density increases, but still reasonable risk profile
- Mature adults (36+): Higher complication rates, more challenging recovery, stronger evidence needed to justify elective removal
A study in the American Journal of Public Health found complication rates nearly doubled after age 35 compared to extraction before age 25, supporting earlier intervention when removal is clearly indicated.
The Monitoring Protocol: When Watching Is Appropriate
For wisdom teeth that don't require immediate extraction, a structured monitoring approach helps detect problems early.
Radiographic Surveillance
Imaging plays a crucial role in third molar monitoring:
- Initial panoramic assessment: Establishes baseline position and development
- Periodic follow-up imaging: Typically every 24-36 months for stable cases
- Cone beam CT: May be indicated for complex positional relationships
- Bitewing extensions: Can help monitor for early decay between second and third molars
These imaging protocols help track changes that might indicate developing problems.
Clinical Examination Elements
Regular dental check-ups should include specific wisdom tooth assessment:
- Probing depths: Measuring the gum pockets around third molars
- Bleeding assessment: Checking for inflammation indicators
- Mobility testing: Evaluating stability within the socket
- Occlusal evaluation: Assessing functional contact and potential interference
- Hygiene assessment: Determining cleaning effectiveness in the third molar region
Deterioration in any of these parameters may indicate a need to reconsider the retention decision.
Patient Self-Monitoring Guidance
Patient Self-Monitoring Guidance
- Persistent soreness: Particularly behind the second molars
- Food trapping: Difficulty keeping the area clean despite good technique
- Swelling episodes: Even if they resolve without intervention
- Taste or odor changes: Indicating possible infection
- Jaw stiffness: Especially upon waking or after long conversations
Early reporting of these symptoms allows for timely intervention before significant complications develop.
Extraction Considerations: When Removal Is the Right Choice
When wisdom tooth extraction becomes necessary, several factors influence the approach and timing.
Optimal Timing Considerations
Research supports certain timing principles when extraction is indicated:
- Root development stage: Ideally performed when roots are 1/3 to 2/3 formed
- Age-related healing: Recovery typically faster and with fewer complications before age 25
- Academic/work scheduling: Planning around recovery time availability
- Seasonal timing: Some evidence suggests slightly better outcomes during lower-stress periods
The International Journal of Oral and Maxillofacial Surgery published findings supporting the "golden period" for wisdom tooth removal between ages 17-25 when indicated.
Surgical Approach Options
Modern extraction techniques offer several approaches based on tooth position:
- Simple extraction: Possible for fully erupted teeth with favorable anatomy
- Surgical extraction: Required for impacted teeth, involving tissue incision and bone removal
- Sectioning techniques: Dividing the tooth for removal in multiple pieces
- Coronectomy: Intentional retention of roots when complete removal poses nerve risk
These techniques continue to evolve, with minimally invasive approaches reducing recovery time and complication rates.
Anesthesia and Comfort Management
Patient comfort options have expanded significantly:
- Local anesthesia: Sufficient for simple cases in comfortable patients
- Nitrous oxide: Provides anxiety reduction while maintaining consciousness
- Oral sedation: Creates deeper relaxation with amnesia effects
- IV conscious sedation: Produces controlled semi-consciousness with excellent amnesia
- General anesthesia: Complete unconsciousness, typically reserved for complex cases
At Vident Dental Clinic, we tailor the anesthesia approach to both the surgical requirements and the patient's comfort needs.
Recovery Optimization: Ensuring Smooth Healing
When extraction is performed, several strategies improve the recovery experience.
Evidence-Based Recovery Protocols
Research supports specific post-extraction approaches:
- Controlled anti-inflammatory use: Scheduled NSAID administration before pain onset
- Ice application: Intermittent cooling during the first 24 hours
- Proper nutrition: Soft but nutritious foods supporting healing
- Gentle hygiene resumption: Careful cleaning around surgical sites after 24 hours
- Activity modification: Gradual return to exercise avoiding pressure spikes
These protocols significantly reduce discomfort and complication rates when followed consistently.
Warning Signs Requiring Attention
Patients should seek prompt evaluation for:
- Excessive bleeding: Saturating gauze after the first day
- Severe pain: Not responding to prescribed medications
- Swelling increase: Particularly after the third day
- Fever development: May indicate infection requiring intervention
- Numbness persistence: Lasting beyond initial anesthetic duration
Early intervention for these signs prevents more serious complications and improves outcomes.
Special Considerations for Unique Situations
Certain circumstances require modified approaches to wisdom tooth management.
Orthodontic Implications
The relationship between third molars and orthodontic treatment remains nuanced:
- Crowding concerns: Limited evidence supporting wisdom teeth as a primary crowding cause
- Orthodontic planning: May factor into comprehensive treatment strategies
- Post-treatment stability: Considerations for retention and relapse prevention
- Space assessment: Evaluation of adequate room for functional eruption
The American Association of Orthodontists position statement indicates that decisions should be made case-by-case rather than automatically extracting for orthodontic reasons.
Medical History Factors
Systemic health conditions influence wisdom tooth management:
- Bleeding disorders: May require specialized protocols for extraction or favor monitoring
- Immunocompromise: Higher infection risk affecting both retention and removal decisions
- Medication considerations: Bisphosphonates, anticoagulants, and other drugs requiring special protocols
- Radiation history: Previous head/neck radiation treatment complicating healing
- Cardiovascular conditions: Requiring specific anesthesia and stress management approaches
These factors necessitate collaboration between dental providers and medical specialists for optimal outcomes.
Pregnancy Considerations
Expectant mothers require special attention:
- Timing options: Second trimester generally safest if intervention needed
- Imaging modifications: Minimized radiation exposure with appropriate shielding
- Medication limitations: Restricted analgesic and antibiotic options
- Position accommodations: Modified chair positioning for patient comfort and safety
- Urgent vs. elective timing: Distinguishing between necessary and deferrable treatment
The American College of Obstetricians and Gynecologists and the American Dental Association provide joint guidelines for managing dental needs during pregnancy.
The Vident Approach to Wisdom Tooth Evaluation
At Vident Dental Clinic, we've developed a comprehensive protocol for third molar assessment that balances current evidence with individual patient factors.
Our Assessment Process
Our evaluation includes:
- Detailed history of previous symptoms or issues
- Comprehensive clinical examination of third molar regions
- Appropriate imaging to determine position and relationships
- Discussion of findings and options with clear visual aids
- Shared decision-making incorporating patient preferences
This thorough approach ensures recommendations based on your specific situation rather than generalized policies.
Our Treatment Philosophy
We emphasize:
- Conservative management when appropriate
- Preventive extraction only when evidence supports likely future problems
- Optimal timing when intervention is indicated
- Comfort-focused approaches to surgical care
- Comprehensive follow-up regardless of the chosen path
This balanced philosophy aligns with current research while respecting patient autonomy in treatment decisions.
Our Commitment to Continued Monitoring
For patients choosing retention, we provide:
- Structured follow-up schedules based on risk assessment
- Clear documentation of baseline conditions for comparison
- Patient education on self-monitoring techniques
- Periodic reevaluation of the risk-benefit balance
- Prompt availability if concerns develop between scheduled visits
This ongoing care ensures that initial decisions can be modified if circumstances change.
Conclusion: Personalized Care for Optimal Outcomes
The days of automatically removing all wisdom teeth are behind us. Current evidence supports an individualized approach that considers the unique characteristics of each patient's third molars, their overall health, preferences, and risk factors.
While some wisdom teeth clearly require removal due to disease, symptoms, or high complication risk, others may remain in place indefinitely with proper monitoring and care. The key lies in thorough evaluation, clear communication about options, and ongoing surveillance for those choosing retention.
At Vident Dental Clinic, we're committed to providing evidence-based guidance tailored to your specific situation. Whether your wisdom teeth require removal, are candidates for monitoring, or fall somewhere in between, our team will help you navigate this decision with the most current information available.
We invite you to schedule a comprehensive wisdom tooth evaluation to discuss your unique circumstances and develop a plan that serves your long-term oral health.
This article provides educational information about wisdom teeth management. For personalized recommendations, please schedule a consultation with our dental team at Vident Dental Clinic.